Commonwealth Minister for Health, the Hon Greg Hunt MP, this week announced the establishment of a new partnership between the Infection Control Expert Group (ICEG) and the Taskforce as part of a broader strategy to help protect healthcare workers from COVID-19.
The Taskforce will establish an Infection Prevention and Control Working Group which will be co-chaired by members of the Taskforce and ICEG. The Taskforce will be working with ICEG over the coming week to identify key areas of expertise required on the Working Group.
The objective of the partnership is to strengthen the evidence-base for national guidance on infection prevention and control-related issues that impact clinical practice, and to work with the broad membership of the Taskforce to strengthen clinical input and generate national consensus on specific infection control questions. Recommendations jointly developed and approved by the Taskforce and ICEG will be submitted to Australian Health Protection Principal Committee (AHPPC) for consideration.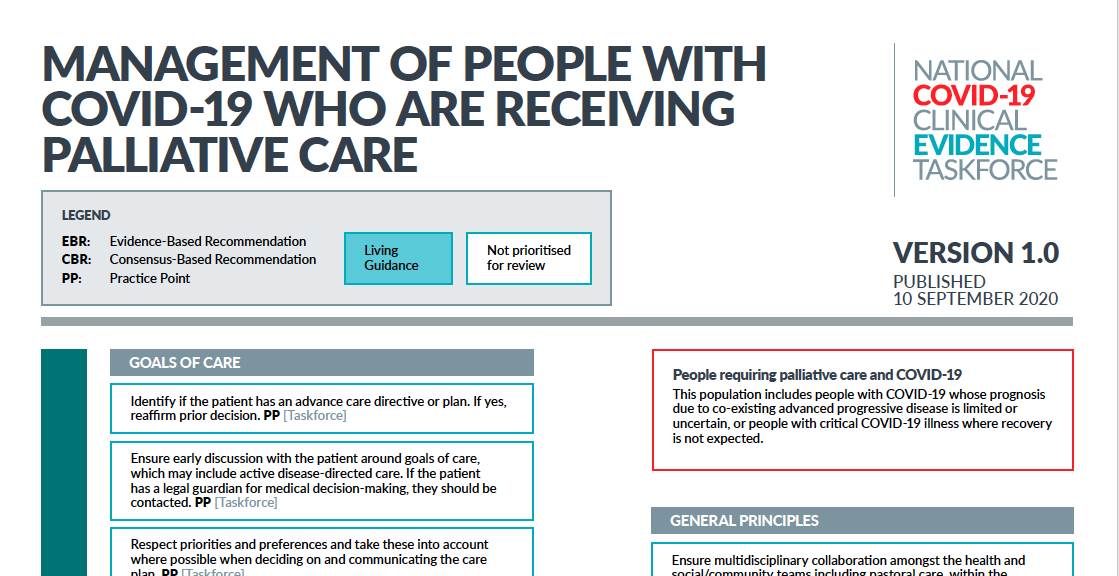
The Care of Older People and Palliative Care Panel has published a clinical flowchart for the Management of people with COVID-19 who are receiving palliative care.
Co-Chair of the Panel, and Chair of Palliative Care Australia, Professor Meera Agar said the guidance has taken into consideration the particular needs and requirements of people facing a life-limiting illness.
“Our advice is based both on Australian and international evidence and will evolve as our understanding of COVID-19 grows. The COVID-19 pandemic has proven that two elements are essential to provide informed care to patients suffering from a new disease: the collaboration of health professionals and researchers, and the development of evidence-based best practices to guide our action.
“I am proud to say we have come together as both researchers and health professionals to determine the best ways to care for people with COVID-19 who are receiving palliative care. As it follows a ‘living evidence’ model, the flowchart may be updated as new research is led and new evidence is uncovered.”
The Disease-Modifying Treatments and Chemoprophylaxis Panel have reviewed two new randomised controlled trials concerning the use of hydroxychloroquine in the treatment of COVID-19 and have made no change to the existing recommendation.
The evidence base has been updated with no change to the strength or direction of the recommendation.
New recommendation
For people with COVID-19, do not use interferon β-1b outside of randomised trials with appropriate ethical approval.
The wording of the recommendation has been changed for consistency with no change to the strength or direction of the recommendation.
For people exposed to individuals with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection, do not use hydroxychloroquine for post-exposure prophylaxis outside of randomised trials with appropriate ethical approval.
The titles have been updated to reflect that neonates are included in the recommendations.
New consensus recommendation
For mechanically ventilated neonates, children and adolescents with COVID-19 and hypoxaemia despite optimising ventilation, consider prone positioning if there are no contraindications.
New consensus recommendation
For mechanically ventilated neonates, children and adolescents with COVID-19 and moderate to severe ARDS with atelectasis, consider using a higher PEEP strategy over a lower PEEP strategy. The absolute PEEP values that constitute a high and low PEEP strategy will depend on age and patient size.
New consensus recommendation
For mechanically ventilated neonates, children and adolescents with COVID-19 and hypoxic respiratory failure characterised by severe atelectasis unresponsive to other ventilation strategies, consider using recruitment manoeuvres.
New conditional recommendation against
For intubated neonates, children and adolescents with COVID-19, do not routinely use continuous infusions of neuromuscular blocking agents (NMBAs).However, if effective lung-protective ventilation cannot be achieved, consider targeted intermittent use of NMBAs. If indicated, the choice of NMBA should be guided by the age group and regional practice.
The section title has been changed from ‘Anticoagulants’ to ‘Venous thromboembolism (VTE) prophylaxis’.
New consensus recommendation
In postpartum women with COVID-19 who have hypertension requiring treatment with ACE inhibitors, there is currently no evidence to deviate from usual care. These medications should be initiated or continued unless otherwise contraindicated.
The evidence base has been updated with no change to the strength or direction of the recommendation.
The Taskforce is continually monitoring research to update recommendations weekly as new evidence accumulates.
Seven clinical flowcharts have been developed by the Taskforce to cover:
Changes to flowcharts this week reflect:
We are currently reviewing evidence to develop recommendations and flowcharts to guide practice in areas including:
Cochrane contributors around the world continue to focus on COVID-19, collaborating in international efforts to understand, contain and stop the spread of coronavirus. Cochrane Australia have prepared a snapshot of this global work to date, along with helpful resources and initiatives now underway.
Cochrane COVID Special Collections:
It is a core mission of the Taskforce to engage with frontline clinicians to rapidly identify and address priority clinical questions.
Each week we collect suggestions for new clinical questions or topics for consideration by the Taskforce. A document that lists all of the suggested questions, topics and new patient groups that we have received to date is available here.
Please encourage your clinical colleagues to provide their insights via the website.